AI in healthcare has moved from promise to practice. Hospitals, health systems, and digital health companies now use it in diagnostics, operations, and patient engagement. The measure of value has shifted to cost reduction, quality of care, and competitiveness.
Radiology teams apply AI to flag urgent scans. Oncologists lean on it to help decide which treatment to go with. Admin teams save time (and a lot of stress) by letting AI handle coding, documentation, and scheduling. Remote care teams use it to keep an eye on patients at home without constantly rushing in.
For leadership, the real challenge is making sure these systems actually scale, plug into everyday workflows without breaking things, and stay on the right side of compliance. That requires seamless integration with existing workflows, strict compliance with regulations, and outcomes that matter to both clinicians and executives. AI is becoming a core driver of efficiency and sustainable growth in healthcare.
Where Healthcare Companies Are Using AI Today
AI in healthcare has moved beyond the lab. It’s reshaping hospital economics by lowering costs, speeding up diagnostics, and enabling new models of care. A few areas stand out:
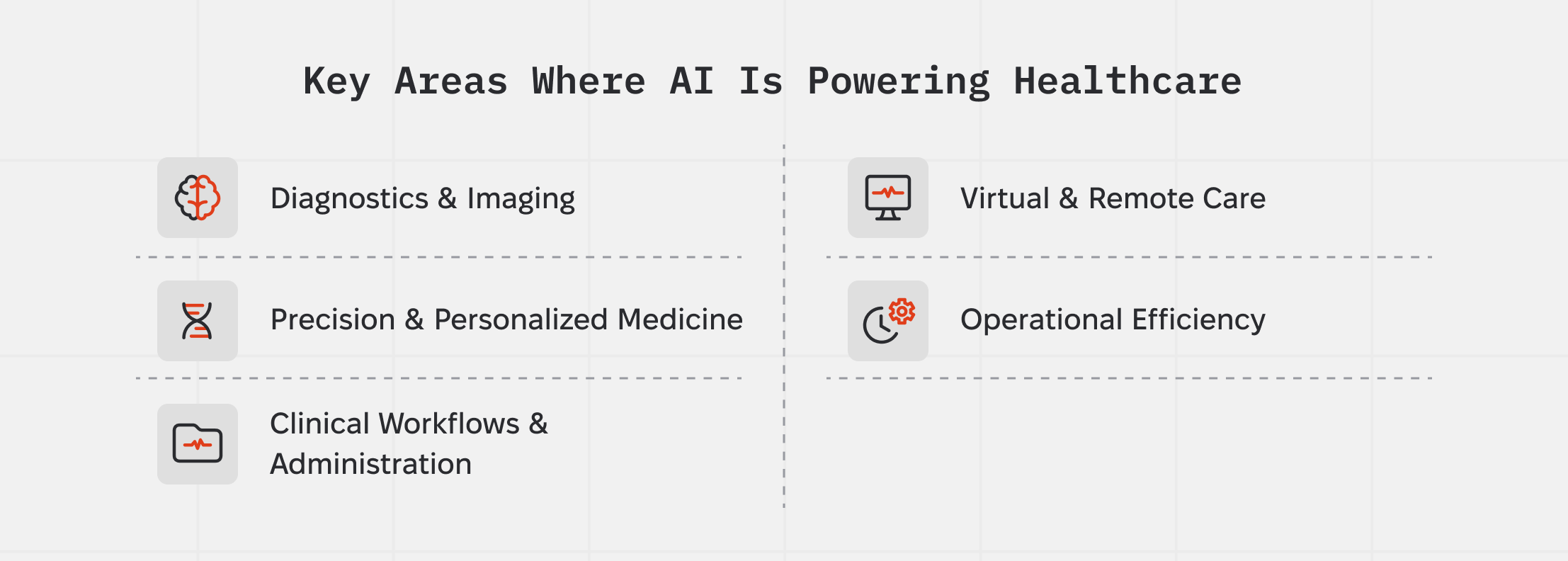
Diagnostics & Imaging
Radiology and pathology are where AI is proving itself fastest. Tools like Aidoc and Qure.ai scan thousands of images a day, flagging strokes or lung issues in minutes — work that used to pile up on already overworked specialists. Pathology is following suit: PathAI uses machine learning to boost accuracy in oncology diagnostics, helping pharma companies cut trial costs and timelines.
Precision & Personalized Medicine
In cancer care, the business case for AI is speed and better outcomes. Tempus analyzes genomic and clinical data to match patients with targeted therapies, giving hospitals a way to offer “big pharma-level” precision medicine in-house. DeepMind’s AlphaFold, meanwhile, has solved protein folding challenges that shave years off early-stage drug discovery..
Clinical Workflows & Administration
AI helps with more than clinical outcomes — it saves time too. Augmedix and Abridge turn doctor–patient conversations into structured notes, cutting paperwork by up to 70%. XpertDox applies autonomous coding to streamline billing, reducing denials and accelerating cash flow. For CFOs and COOs, this is where healthcare AI makes a direct impact on revenue cycles.
Virtual & Remote Care
The economics of home healthcare are shifting. Cera uses AI monitoring to reduce hospital readmissions, positioning itself as a cost-saver for payers and providers. K Health scales virtual triage by analyzing millions of anonymized health records, giving patients instant access to AI-backed primary care. Sword Health blends AI and human therapists to deliver musculoskeletal care remotely — a market worth billions given the burden of chronic pain.
Operational Efficiency
Finally, AI is tackling back-office headaches. Hospitals use predictive scheduling to cut overtime costs and supply chain algorithms to anticipate shortages before they hit operating rooms. For executives, these gains are often the quickest path to ROI because they don’t require clinical approval or patient adoption.
What We Can Learn From Market Leaders
The companies moving healthcare AI forward keep technology tied to business goals. Their track record gives executives a few clear lessons: make sure AI fits into daily workflows, connect the data, automate where labor costs sting the most, and set up governance that people can actually trust.
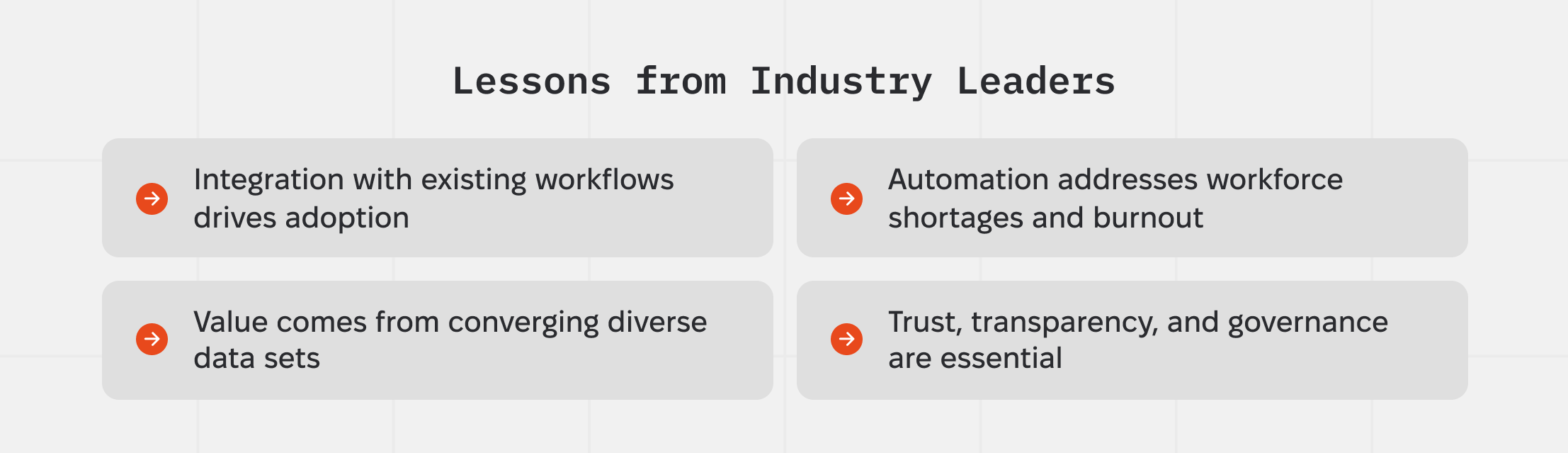
Integration with existing workflows drives adoption
Deployments that “snap into” current practice see faster uptake and scale. Example: Aidoc’s platform rolled out across 13 hospitals at University Hospitals, embedding into existing radiology and care pathways rather than adding extra steps. Ambient documentation tools show similar traction when launched inside normal visit flows; multi-site results (Mass General Brigham, Emory) link ambient tech to lower documentation burden and clinician burnout.
Value comes from converging diverse data sets
Leaders invest in multimodal data (genomics + clinical + imaging) to unlock decisions that point-solutions can’t. Tempus is building a large multimodal foundation model with AstraZeneca and Pathos and is integrating its AI co-pilot directly into Northwestern Medicine’s EHR—data + workflow together is the pattern.
Automation addresses workforce shortages and burnout
With a projected U.S. physician shortfall of up to 86,000 by 2036, automating documentation, coding, scheduling, and prior auth is a financial imperative, not a convenience. Ambient tools and AI scribes show measurable reductions in documentation time and after-hours work in recent studies.
Trust, transparency, and governance are essential
Systems that scale AI start with governance: transparent model claims, monitoring, and change control. The Coalition for Health AI “Blueprint for Trustworthy AI” lays out practical assurance and reporting guidance specific to healthcare. ONC’s HTI-1 rule adds transparency requirements for decision-support algorithms in certified EHRs, and the FDA’s 2025 draft guidances (AI-enabled device lifecycle and PCCP) clarify expectations for safety, effectiveness, and model updates.
Market Gaps and Untapped Opportunities
Healthcare AI has advanced quickly in diagnostics and imaging, but several high-value areas remain underserved. These aren’t abstract challenges—they’re measurable cost centers where providers, payers, and health systems are still bleeding money. Closing these gaps could unlock the next wave of efficiency and growth.
AI for Revenue Cycle and Reimbursement Complexity
While most attention in healthcare AI goes to imaging or diagnostics, the financial side of medicine remains under-served. Providers lose an estimated 3–5% of net patient revenue to denied or incorrectly coded claims. For a mid-sized hospital, that can mean millions in preventable losses each year. AI tools that predict denials before submission, generate automated appeals, or cross-check coding against payer rules could plug one of the biggest revenue leaks in the system.
AI for Staffing and Workforce Optimization
Labor is the single largest expense in healthcare, accounting for more than 50% of hospital operating costs. Burnout and staffing shortages have made workforce planning unpredictable, forcing hospitals to rely on costly agency staff. While AI has helped automate documentation, very few solutions target predictive scheduling, workload balancing, or real-time nurse reallocation. Vendors who can apply AI to workforce management stand to deliver cost savings at a scale larger than most clinical tools.
AI for Supply Chain Resilience
The pandemic exposed how fragile hospital supply chains can be. Surgeries were delayed or canceled because basics like gloves, masks, and common drugs ran short. Supply chain AI still feels niche, often tacked onto old ERP systems, leaving big gaps in forecasting, demand sensing, and supplier risk checks. Even preventing a small number of canceled procedures can protect patient outcomes and save hospitals millions.
AI for Preventive and Chronic Care Management
Acute care may grab headlines, but ninety percent of the nation’s $4.9 trillion in annual health care expenditures are for people with chronic and mental health conditions. Despite this, most AI investment flows to radiology or oncology, not diabetes, COPD, or mental health. The opportunity lies in building AI tools that flag early risk, support long-term adherence, and predict relapses before costly hospitalizations. For payers and providers in value-based care models, prevention is not just good medicine—it’s a bottom-line necessity.
Conclusion & Takeaways
AI in healthcare has become part of the backbone for hospitals and health systems. The ones making headway are folding it into day-to-day work so things run faster, more accurately, and without piling on extra cost.
The next stage of growth will come from solving unaddressed but valuable problems: connecting fragmented data, strengthening chronic and preventive care, and creating tools that mid-sized providers can both afford and deploy.
For innovators, the ask is simple on paper but tough in practice: design with integration and compliance in mind from the start. For investors, the better move is to back companies that figure out scale, reimbursement, and everyday efficiency.
AI will earn its place by showing real results in the spots where hospitals feel the most pressure.





.png)

.webp)




